England, After the Smoke
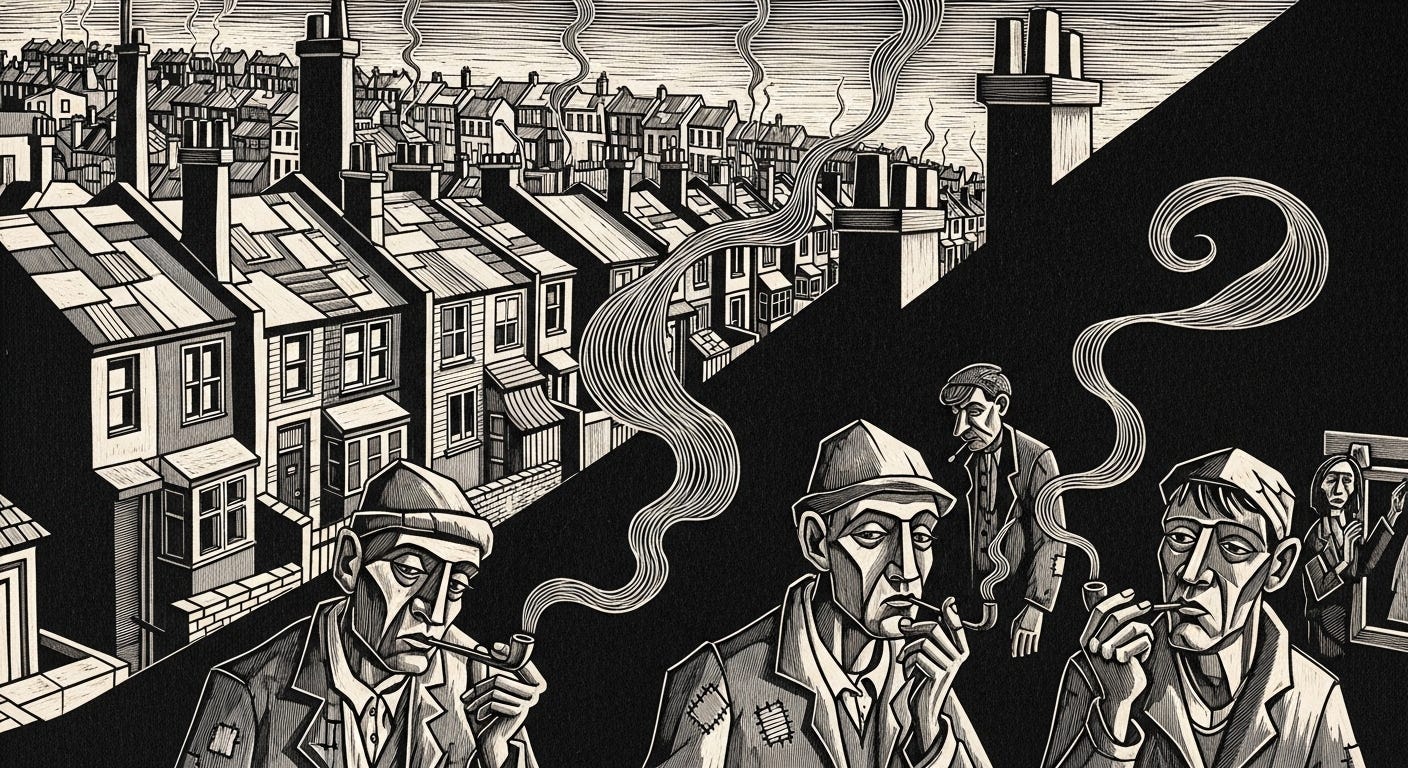
Cigarettes are receding, but the air remains heavy with deeper dilemmas: pleasure, risk, and control.
Smoking is declining, vaping is rising, and the science is clear. Yet Britain’s response remains trapped between moral anxiety and political caution. Harm reduction is advancing in bodies and communities, but still faltering in policy, language, and power.
There are moments when data do more than inform: they shift the ground beneath public debate. They do not merely add nuance; they rupture consensus, erode certainties, and force repositioning.
The newly released Health Survey for England: 2024 marks one of these rare inflection points. Smoking in England has fallen to its lowest level since records began: just 11 percent of adults identify as smokers, a proportion that, according to the survey itself, continues on a downward trajectory.
As combustible cigarettes retreat, the use of electronic nicotine devices moves in the opposite direction.
E-cigarettes now reach 10 percent of the population, with the steepest increase among young people aged 16 to 24. In this age group, vaping has ceased to be an exception and has become a declared habit: 19 percent of women and 16 percent of men report current use.
The numbers speak. But it is when they seem to whisper that they announce the most profound changes.
At first glance, all this may appear to be little more than a shift in habit, a behavioral detail, almost cosmetic. But data rarely settle for the surface. They move faster than the policies that attempt to keep pace with them, exposing a deeper sociopolitical, ethical, and epistemological realignment.
“We are seeing patterns of nicotine use change across the entire population,” says Cliff Douglas, former vice president of the American Cancer Society and a central figure in the shaping of contemporary tobacco-control policy.
“The most telling data point is that e-cigarette use among adults who have never smoked remains very low. That points less to the emergence of a new epidemic and more to a movement toward risk reduction among smokers.”
What transforms the body almost always precedes what transforms the law.
Douglas’s reading gains substance in a figure that demands silence before interpretation: only 4 percent of adults who have never smoked report currently using vapes.
At the same time, vaping is advancing precisely where cigarettes still cling to life and where life itself is harsher. In the poorest areas, 13 percent of adults have adopted these devices, compared with just 7 percent in the wealthiest regions.
This is not merely a trend or a generational whim. It is a survival strategy in landscapes shaped by precarity: places where health is an intermittent luxury and relief an everyday urgency. In these territories, each inhale is also a pause from pain. These, too, are data.
“If it weren’t for the moral panic surrounding e-cigarettes, many more vulnerable people would already have managed to quit smoking,” says Louise Ross, former director of the Leicester Stop Smoking Service and one of the pioneers of a vape-friendly approach within Britain’s public health system.
“Instead,” she reports, “we repeatedly hear people say, ‘At least with cigarettes, we know what’s in them.’”
“That is misinformation,” Ross concludes. “And it costs lives.”


The idea of harm reduction is not new. But in light of the evidence, it has become inescapable. The data reveal what many authorities still hesitate to admit: a growing share of the population is abandoning a demonstrably lethal product for another that is significantly less harmful, despite institutional reluctance, ambiguous or openly adversarial public messaging, and a regulatory framework that oscillates between delay and fear.
The war on smoking, which at many moments spilled over into a war on nicotine itself, now demands more than statistics. It demands a direct confrontation with misinformation and paternalism that deny informed choice; with a morality disguised as care; and with a public language that clings to abstract ideals even when the cost is concrete, measurable, and real.
Nicotine persists. Cigarettes, perhaps not.
But the air still carries ghosts.
And the state, its interests and its vices.
What is at stake is whether policy will continue to fight substances or finally begin to protect people.
The Data Breaks the Silence; and Panic Intervenes
Almost without fanfare, the Health Survey for England: 2024 was released by the National Health Service on January 27. It is an extensive survey, with regional reach and a validated methodology, one of those bureaucratic instruments that seem cold until, when read closely, they begin to reveal human warmth.
Seen up close, the report functions like a silent seismograph: it does not announce earthquakes, but it repositions the country from within, capturing shifts in bodies, in repeated gestures of consumption, in routines of risk, and in the often discreet forms of survival that shape the lives of the British population.
Among dozens of tables and charts, two figures interrupt the reading. Not because of their magnitude, but because of the friction they produce. Eleven percent of adults in England still smoke, the lowest rate ever recorded. Ten percent now use e-cigarettes. For the first time since the series began, the country has nearly as many vapers as smokers.
This is not a statistical coincidence but a historic inflection point. For more than a century, combustion served as nicotine’s primary vehicle, but it is now losing its hegemony to vapor: adjustable, customizable, flavored. A technology of consumption that is not merely technical but also a language, a market, and a field of dispute.
At first glance, this may seem like a simple exchange of habits. But beneath the gesture, that almost unconscious motion of bringing something to the lips, the grammar of pleasure and risk shifts. The cigarette, once an emblem of rebellion and status, of addiction and a rite of passage, is becoming an exception: a custom retreating to the margins. In its place, another form of consumption, more discreet, flavored, and customizable, emerges, appearing with increasing frequency precisely among those whom conventional cessation campaigns have rarely managed to reach.
This, however, is no pure or uncomplicated triumph. The transition now underway, from combustion to vapor, is crossed by tensions between health and market, science and morality, and risk and pleasure. Even so, one fact remains unavoidable: harm reduction is occurring, with or without the blessing of authorities. And perhaps, increasingly, despite them.
The British Paradox: From the Harm Reduction Lab to the Theater of Containment
For more than a decade, the United Kingdom stood as a global reference for tobacco harm-reduction strategies. In 2015, a formulation by Public Health England helped redefine the international debate by stating that vaping was substantially less harmful than smoking, an estimate distilled into a phrase that circled the world: “vaping is 95% less harmful than smoking.”
From that point on, the country adopted an explicitly pragmatic, evidence-based approach. Vapes were distributed in hospitals, incorporated into smoking-cessation programs, and promoted in public campaigns as an alternative to cigarettes.
And the results did not take long to appear.
According to the Office for National Statistics, the proportion of smokers declined from 17.2 percent in 2015 to 12.9 percent in 2022. A sustained decline, and a rare one among high-income countries. But this model began to wobble in 2025, when policy became increasingly captured by the dramaturgy of fear.
In August of that year, The Guardian published an alarmist report claiming that young people who used vapes were “three times more likely” to start smoking, alongside a list of alleged risks: asthma, depression, and mental disorders.
The article acknowledged that the evidence was observational and incapable of establishing causal relationships. But the media framing had already done its work.
Under pressure from the media and from the political and discursive ecosystem surrounding the World Health Organization, the British government fast-tracked the Tobacco and Vapes Bill. The response included a ban on disposable vapes, severe limits on flavors, and standardized packaging. The tone was one of alarm: media spoke of a “youth nicotine epidemic”, a phrase that mobilized moral anxiety far more than it rested on consistent empirical support.
A country that, for years, had led innovation in public-health policy was now legislating in a reactive mode, responding as if to chaos, despite a robust domestic scientific literature and data pointing in the opposite direction.
One example is telling. The Health Survey for England: 2024 shows that only 4 percent of adults who have never smoked report current vape use. Among children aged 8 to 15, just 2 percent say they have ever tried conventional cigarettes, while 9 percent report having experimented with vapes at least once. A relevant difference, but one that does not amount to regular use, nor to a transition into smoking.
Far from signaling a new generation of dependents, these figures suggest a shift in the initiation pathway: the cigarette has lost its historic role as an entry rite. Nicotine now arrives through a more discreet route that is substantially less toxic and, to date, after roughly two decades of population-level use, has not been consistently linked to direct lethality.
And perhaps that alone already constitutes a silent achievement.
Professor Ann McNeill, an expert in nicotine dependence at King’s College London, publicly challenged the scientific foundations of the new legislation. In her analysis, 53 of the 56 systematic reviews used to justify the restrictions were classified as being of “low” or “very low methodological quality.”
The error, she argued, was elementary: confusing association with causation, reading correlation as destiny.
The paradox is plain: where vaping rises, smoking continues to fall.
Even so, evidence was overrun by rhetoric. In the name of protecting young people, the risk is punishing those who have finally found a less lethal route of escape. The NHS, meanwhile, continues to support vaping as an effective cessation tool, backed by systematic reviews from Cochrane.
In Westminster, however, political alarm intensifies. The country that once served as a laboratory for harm reduction now hesitates despite its own evidence.
‘Nicotine Doesn’t Kill; Moralism Might.’
Part of the regulatory impasse and the social noise surrounding vaping stems from a persistent semantic confusion that has cost public health decades: treating nicotine and cigarettes as synonyms.
It is combustion, not the substance itself, that constitutes the lethal axis. Tobacco smoke contains roughly 7,000 chemical compounds, at least 70 of which are known carcinogens. By contrast, nicotine is not the agent responsible for cancer, heart attacks, or chronic obstructive pulmonary disease, the principal lethal outcomes associated with smoking.
This does not mean nicotine is free of physiological effects. It means nicotine does not explain the mortality associated with smoking. What nicotine produces, above all, is dependence. And dependence, though frequently conflated with addiction, is not, by definition, synonymous with destruction.
Clinically, addiction severely compromises autonomy, functioning, and physical or mental health. By contrast, dependence can be stable, functional, and—in many contexts—socially integrated, as with caffeine, certain antidepressants, long-term controlled use of benzodiazepines, or even regulated sugar consumption.
In the case of nicotine, the decisive difference lies in the mode of delivery. A cigarette delivers the substance abruptly, along with a toxic cocktail generated by combustion. By contrast, vaping allows greater dose control, intermittent use patterns, and a lower associated physiological burden. The same applies to pouches, gums, patches, and oral sprays. Yet precisely because vaping is effective, pleasurable, and popular, it has become the primary target of public suspicion.
As Cliff Douglas, one of the most influential figures in contemporary tobacco regulation and a global reference in public health, puts it:
“Nicotine doesn’t kill—smoke does.”
Douglas, a trained jurist, devoted more than three decades to tobacco regulation. He led historic campaigns, including the ban on smoking on commercial flights in the United States, and played a central role in defending Uruguay against Philip Morris’s attempt to overturn Uruguay’s public-health laws.
For him, Britain’s progress in reducing smoking rates is inseparable from access to less harmful products.
“Smoking rates continue to fall in England and are now at record lows, thanks in part to the substitution of vaping products for combustible cigarettes,” he said in an interview.
“What is most striking,” he adds, “is that vape use among adults who have never smoked remains very low. This shows that we are not creating a new epidemic but rather accelerating smoking cessation among the most vulnerable.”
That vulnerability, moreover, has been intensified by a cruel paradox: by demonizing nicotine, policy perpetuates the consumption of its most lethal form—the cigarette—among the poorest.
This is precisely what Louise Ross, one of the most respected voices in smoking cessation in the United Kingdom and a leading authority on harm reduction, has warned against. A nurse by training, Ross spent years on the front lines of Britain’s public health system.
Now leading the Stop Smoking initiative at Smoke Free Digital, she became a firm advocate for safe substitution through direct clinical experience: over time, she observed consistently higher quit rates among smokers who combined vaping with structured clinical support.
“The scare stories around vaping have created a perverse effect,” Ross says. “People in vulnerable situations end up saying, ‘At least with cigarettes, we know what’s in them.’ That is a direct result of misinformation—including from health professionals.”
For Ross, nicotine should be treated with the same level of rationality applied to other substances used chronically.
“The central goal is to be free from smoke, not from nicotine. Gradual reduction is possible, yes—as long as it is voluntary, not punitive. What we cannot do is force abstinence in the name of an abstract purity and, in doing so, push people back toward cigarettes.”
The history of nicotine may need to be retold. Not as the story of a vice, but as a poorly told chronicle of misplaced focus. By demonizing the substance, we ignore the true vector of harm and, in doing so, forfeit a concrete chance to save lives.
Care, in this case, begins with an increasingly rare gesture: the political humility to listen to data before obeying instinct.
The Uneven Geography of Combustion
Not every decline is uniform. If the smoking curve plunges in the aggregate, it stumbles at the margins. There are territories where the cigarette still endures as a symptom of inequality, abandonment, and absence, not as a choice.
And it is precisely in these interstices that vaping begins to seep in, not merely as a technological promise but as a possible form of relief. A smoke-free future may be arriving. But, as always, it does not arrive at the same time for everyone.
The historic decline in smoking in England from nearly 30 percent in the early 2000s to 11 percent in 2024 marks an undeniable public-health milestone. However, this achievement has not been distributed evenly.
In the wealthiest neighborhoods, where access to information, time, and care is less fiercely contested, cigarettes have all but vanished: only 7 percent of adults still smoke. In poorer communities, however, the rate more than doubles, reaching 17 percent. Among men in the most vulnerable circumstances, the rate rises to 20 percent, nearly three times that of men in the highest income brackets.
In these territories, combustion is more than a habit: it is a symptom. A visible marker of chronic stress, accumulated exclusion, and scarcity of viable alternatives. Lighting a cigarette in the Northeast of England or in working-class neighborhoods of Yorkshire is not merely an act of nicotine consumption. It is a form of coping. For many, it is the only constant in lives shaped by uncertainty.
It is precisely in these same territories that vaping is growing most rapidly.
In poorer areas, 13 percent of adults now use e-cigarettes, almost twice the rate observed in more affluent regions, where the figure stands at 7 percent.
The contrast reveals more than a simple technological substitution. It suggests that vaping is filling a void left by traditional cessation campaigns, or perhaps by the NHS finally getting it right. In places where cigarettes persist as a cultural and affective marker, electronic devices offer an escape: for many, partial and imperfect, but concretely real.
This is the side of the statistics that rarely makes headlines. In these territories, vaping is neither an adolescent fad nor a marketing ploy. It is a survival strategy, a substitute that, even without the sheen of novelty, promises less pain, less disease, and less loss. As one expert quoted in the NHS survey put it: “We may be winning the war against cigarettes at the national level, but not everyone is reaping the benefits of that victory.”
Ignoring this asymmetry repeats a familiar error: designing universal policies for a structurally unequal reality. If nicotine has ceased to mean combustion, care, too, must cease to mean command. It must become listening to recognize that, at the margins where embers still glow, vapor may not be a threat but a relief.
The New Moral Anxiety
If, at the margins, the cigarette endures as shelter, at the center, it disappears as a symbol. Among the young, the rite has lost its ritual. For decades, the traditional cigarette played a precise symbolic role: it was the rite of passage of British adolescence. The first drag behind the school. The gesture copied from parents or idols. The smell as a social signature.
In 1997, 19 percent of children ages 8 to 15 had already smoked. Today, that number has fallen to 2 percent. The drop is so steep it borders on the improbable, yet it is, in fact, historic. By contrast, 9 percent of children in that same age group report having experimented with an e-cigarette.
The inversion is evident, but it does not point, as many assume, to a simple substitution of addiction. What is underway is a shift in form, aesthetics, and language. Embers have been replaced by vapor. The ritual has been redesigned.
Instead of an object that betrays itself through smell, color, and stigma, the vape is discreet, flavored, and customizable. It fits both in the pocket and in the imagination of a generation raised under the hegemony of public health and the permanent surveillance of behavior.
“Vaping is now the dominant form of nicotine use among young adults in England,” a consumer said, citing the 2024 data. The survey confirms it: among those ages 16 to 24, 19 percent of women and 16 percent of men report current e-cigarette use—more than double the national average. In contrast, cigarettes are no longer even the predominant option in this age group: only 10 to 11 percent still smoke.
These numbers reveal more than preferences. They cross ethical and political thresholds, posing an uncomfortable question:
What, precisely, unsettles us about youth vaping?
Is it the presence of nicotine or the absence of visible punishment?
Is it fear of a real addiction, the risk of dependence, or discomfort from a form of pleasure that escapes adult control?
Throughout 2025, this anxiety took on institutional form. As noted earlier, the British government subverted its own evidence-based logic and proposed one of the most restrictive legislative frameworks in Europe, including a ban on disposable vapes, severe limits on flavors, and standardized packaging.
The official justification, as always, was the protection of young people. But the rhetorical operation suggests another impulse: a return to performative prohibitionism, in which legislation serves less to reduce harm than to reaffirm authority.
The central question, however, has already been partially answered by Britain’s sociopolitical experience and scientific production: how to protect without punishing? How to craft policies that recognize risk, user agency, social context, and the value of pleasure?
For if the cigarette was long a symbol of transgression, the vape may now be a symbol of ambivalence. And ambivalence demands a more sophisticated vocabulary than the old binary of health and danger.
The United Kingdom does not lack evidence. It lacks political coherence.
A Statistical Victory Is Not Yet an Ethical One
Crossing a threshold is not the same as reaching a destination. If cigarettes no longer occupy the center of nicotine consumption, what remains to be decided is what will take their place: science or fear, evidence-based policy or moral reflex.
The data no longer allows for ambiguity. Vaping has become the primary tool for smoking cessation in the United Kingdom. What is increasingly evident is the absence of a policy that clearly and courageously recognizes this fact.
In 2024, when England recorded—for the first time—more vapers than smokers, the country did more than update its statistics: it turned a page. What remains open is what will be written next.
The traditional cigarette no longer dominates bodies or culture as it once did. Yet it still burns at the margins, among the poor, the underserved, and those forgotten by public campaigns. Its disappearance is uneven. What persists is residual combustion, sustained by timid policies, durable stigmas, and a refusal to treat nicotine with the complexity it demands.
Each year, 28.6 billion cigarettes are consumed in the United Kingdom. More than a statistic, this number is a portrait of persistent inequality and of a dependence perpetuated by policies that still hesitate between care and control.
As a compelling study by Jamie Brown, Sarah Jackson, Sharon Cox, and Vera Buss of University College London has shown, the cigarette persists not because of ignorance but because of institutional inertia.
It has become a zombie product: clinically obsolete yet economically sustained. It remains lit out of convenience and continues to kill through omission. Vaping—imperfect and uneven as it may be—represents a concrete step toward genuine risk and harm reduction.
A step that requires neither perfection nor purity, but political courage: legislating on the basis of science, listening to those who produce evidence and those who use nicotine, and recognizing that pleasure, desire, and need are also components of health.
England is winning the battle against combustion, but it has not yet overcome moralism. Nicotine remains, and with it comes a political challenge: to protect without punishing, to inform without manipulating, to care without prohibiting.
The error now would be to confuse victory with an ending.
No statistic can replace the work of listening. No ban can compensate for the absence of the right to know, choose, and use with lower risk. The only policy that works is one that begins with humility in the face of real life.
As the Canadian physician and writer Mark Tyndall reminds us, “the fight against tobacco is not only a public health challenge—it is an urgent matter of social justice.”
The future of public health may depend less on vertical prohibitions than on an ethic of trust, one that recognizes that, when faced with the choice between smoke and vapor, it is the state’s responsibility to ensure the conditions under which people can decide clearly, justly, and without fear.







Another great essay Claudio. But I must take you up on a point of disagreement. I hate the word 'dependence', not because it is wrong, but because it medicalizes behavior and puts it under the purview and control of public health. I think of my lifetime use of nicotine as a habit: not because it is something distinct and different to dependence, but because habit is an ordinary description of behavior that sits outside of public health purview and control.
Vaping - along with many other behaviors - will never escape the control of public health until such time as we resist and reject the medicalization of our lives.